Recent data from China’s Center for Disease Control and Prevention (CDC) highlights a substantial increase in the prevalence of HIV/Aids in the country over the past two decades, primarily attributed to improved treatment options and enhanced access to testing.
The data, released in October, reveals a remarkable shift in the reported cases of HIV/Aids from 2002 to 2021, with the prevalence rate soaring from 1.09 per 100,000 people to 79.62, a staggering surge exceeding 7,000%. The improvements in treatment and broader testing availability have notably contributed to the marked rise in prevalence, despite an initial increase in the mortality rate associated with HIV/Aids.
Between 2002 and 2018, the mortality rate for reported cases climbed from 0.07 per 100,000 individuals to 1.31 in 2018. However, it has since slightly receded to 1.28 per 100,000 people in 2021.
With more than one million individuals in China living with HIV/Aids, the CDC researchers suggest that China’s comprehensive strategy for HIV/Aids prevention and control, along with its impact on pandemic control efforts, has played a pivotal role in diminishing incidence and mortality rates.
Nonetheless, additional research paints a more challenging picture regarding the pandemic’s effect on HIV outcomes. A study conducted earlier this year found a 14% increase in the yearly mortality rate for HIV in 2020-2022 compared to 2015-2019. The researchers identified the disruption of access to life-saving HIV drugs during the Covid-19 outbreak as a contributing factor.
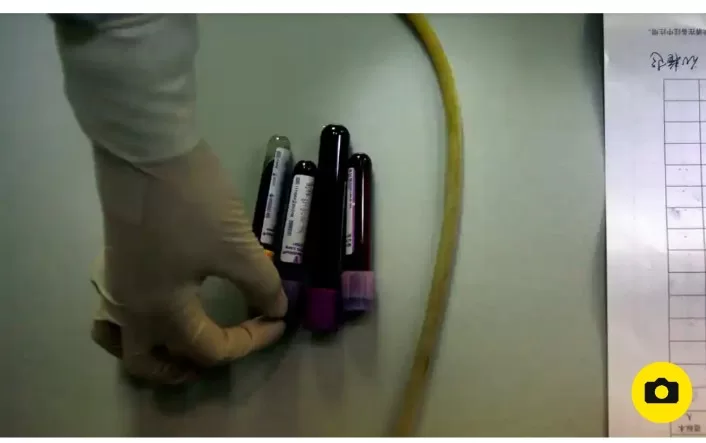
One area where China has made significant progress is in HIV testing. Annual testing surged from 45 million to 200 million between 2008 and 2018, as the country aimed to meet the UN target of 90% of people with HIV knowing their status by 2020. The prevalence of affordable, discreet at-home test kits, largely accessible through China’s massive e-commerce industry, has also contributed to increased testing rates, particularly among high-risk groups.
Nonetheless, recent concerns have arisen due to Beijing’s tightening control over civil society, particularly targeting LGBT+ groups, which has hindered public health workers’ ability to reach these at-risk populations. Medical sociologist Chuncheng Liu emphasized that public health officials cannot fully substitute the crucial role of community organizers and the trust placed in peers within these communities.
The availability of HIV prevention methods such as pre-exposure prophylaxis (PrEP) remains limited in China. PrEP significantly reduces the risk of contracting HIV through sexual contact but is only used by approximately 6,000 individuals, despite receiving approval in 2020.
The data and research reflect the dynamic landscape of HIV/Aids in China and the ongoing efforts to address and control the disease.